Deep Vein Thrombosis (DVT), Deep Vein Narrowing/Occlusion, and IVC Filter Treatments
The Interventional Radiology team at Rochester Regional Health offers minimally invasive treatments for deep vein thrombosis (DVT) as well as all other venous conditions, including deep vein narrowing/occlusions, clot extraction, pulmonary embolus (PE) treatments, as well as inferior vena cava (IVC) filter placement and retrieval.
If you were previously diagnosed with a DVT in the past or having been living with symptoms and issues from them, we will be happy to schedule a consultation to see if we can diagnose or treat you.
The following list is an example of the simple and more complex deep venous diseases we treat with minimally invasive procedures in our Rochester Regional Health Interventional Radiology division:
- Acute DVT clot removal (thrombolysis and thrombectomy)
- Angioplasty and stenting for chronic DVT
- Stenting for May Thurner Syndrome
- Venous reconstruction for chronically occluded veins from prior DVT
- Stenting for Nutcracker Syndrome
- Thrombolysis and stenting for venous thoracic outlet syndrome
- IVC filter placement
- IVC filter retrieval (both routine and complex/high risk retrievals)
- Removal of acute PE from the lungs (thrombolysis and thrombectomy)
What is Deep Vein Thrombosis (DVT)?
Your deep veins carry blood back to your heart from all parts of the body. Deep vein thrombosis (DVT) is the formation of a blood clot (known as a thrombus) in a deep vein, most commonly one of the veins in the leg. In the United States alone, 600,000 new cases are diagnosed each year. A DVT can form in a vein for various reasons, including the following:
- immobility (not moving for an extended period, such as during a long plane or car ride or after a surgery)
- injury to the vein or surrounding tissue
- cancer, even in other parts of the body
- excessive blood clotting, possibly secondary to an inherited condition
- blood clot in a varicose vein extending to a deep vein
Typically, when a blood clot, or DVT, forms in a leg vein, it will either slow down or stop the flow of blood returning from that vein. This is similar to an accident on a highway slowing down or stopping traffic, depending on its severity and extent. If this occurs below the knee, where there are multiple veins returning flow, it will often cause minor symptoms and may resolve on its own. In some situations, it may require the patient taking a blood thinner to help resolve the clot. This is like a major road having an accident, but other nearby roads still being open.
For other DVTs that occur above the knee, or which have extended from a calf vein DVT into a thigh vein or the pelvis, the symptoms are typically worse as there is generally only one major vein returning the flow. This is similar to a highway having a major accident, slowing down flow to a single lane or even stopping traffic completely. Obviously, these blood clots are much more serious and will require blood thinners to help to resolve the DVT, and for most patients a course of blood thinners will suffice.
Besides propagating up the leg veins into the pelvis and abdomen, the other big risk is that a blood clot can break off and travel up the body and lodge in the lung vessels, called a pulmonary embolism, or PE. A PE can be life-threatening in certain situations, and as such is considered an emergency. Thus, the blood thinner is meant to help stop the spread of clot and to prevent a PE from occurring. For certain people who are at a high bleeding risk or for whom blood thinners fail, a device called an IVC filter can be placed in the main vein of the abdomen called the inferior vena cava to prevent the clot from reaching the lung. Filters are a great option for short-term protection, but recent literature has suggested that these IVC filters should be removed whenever possible.
The last issue with DVTs is that even when treated, some large ones will have residual clot in the vein, causing chronic occlusion or narrowing. This results in post-thrombotic syndrome (PTS), which is manifested by a patient constantly feeling the leg with the prior DVT being swollen, aching, throbbing, heavy, and tired, and never fully recovering from the insult of the DVT. Some people will even develop skin darkening, hardening, and/or skin breakdown called ulcers due to poor venous circulation. To prevent this, for some large DVTs that spread up to the pelvis and higher, in addition to anticoagulation certain patients may need the clot to be dissolved (thrombolysis), broken up (angioplasty), extracted (thrombectomy), and/or the vein to be stented open to allow for venous flow to return.
DVT Symptoms
Typical leg deep vein thrombosis (DVT) symptoms include the following:
- Pain or tenderness in the calf or leg (worse with movement or stretching the muscles)
- Redness or discoloration
- Swelling of the leg
- Warmth in the affected limb
- Leg fatigue
DVT and PE Thrombolysis and Thrombectomy
For certain extensive DVTs and PEs which are causing symptoms that could threaten a limb or are excruciatingly symptomatic, our IR team has extensive experience in removing this clot during a single session or staged procedures. Thrombolysis refers to using special clot-busting medications to ?melt away? an acute clot, while thrombectomy refers to physically removing the clot through minimally invasive means.
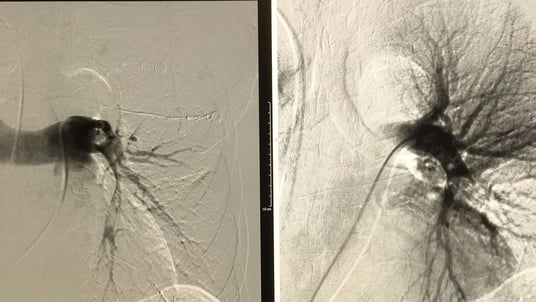
Venous Stenting and Reconstruction
Patients often present with old (or chronic) clots or other causes of narrowing that significantly impede return of venous blood flow. Many patients have compression of the left common iliac vein by the overlying artery, potentially causing significant pain and swelling, called May Thurner Syndrome. Some patients have narrowing, or stenosis, due to chronic old DVT, while others are born without good venous flow.
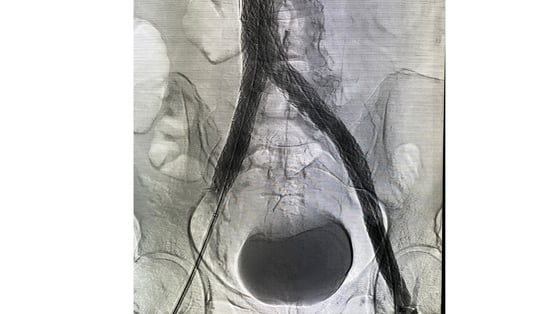
IVC Filter Placement and Retrieval
Often used if you cannot take medications to thin your blood or if you develop blood clots when taking blood thinners or for a more preventative role in high risk patients, inferior vena cava (IVC) filters prevent blood clots from moving from the vein in your legs to the lung (called a pulmonary embolism, or PE).
Placed using a minimally invasive procedure, the vena cava filter is inserted through a catheter via a vein in your groin or neck, and then deployed into the largest vein in your abdomen, the inferior vena cava. Once placed, the filter catches clots that may have potentially broken off and prevent a potential PE.
IVC filters are either “retrievable” (most placed after 2005), which means they are made to be taken out if possible, or “non-retrievable” (most placed before 2005), meaning they were placed as a permanent implant. Over time, these filters may tilt, migrate, or potentially fracture, and thus whenever possible it is recommended that retrievable filters be removed, ideally within the first 6-12 months or whenever safe. If you have an IVC filter, even if you are unsure of how long it has been in or what type, we will be happy to see you in consultation to determine whether removal is best for you. Our IR physicians also have experience with complex filter retrieval, meaning filter that have been for an extended period or which have already moved or changed in some way, making their retrieval more challenging.